The Danger of ‘Feeling Safe’: Long Covid and the Return of Psychosomatic Medicine
Unpacking Sarno’s TMS Theory and Its Quiet Influence on Long Covid Narratives
Cognitive Therapies Part Three
We hope you enjoyed and found some clarity in Parts One and Two of our cognitive therapies series. It’s taken us a little longer to get Part Three out - but huzzah, enough spoons are finally in the cutlery drawer.
In the first article, we took a zoomed-out approach to cognitive applications in chronic illness, and the impact of the industrial mindfulness complex and its numerous systemic and personal issues. Number two lasered in on mind-body medicine with a special focus on the SIRPA conference and Paul Garner. In this edition, we wanted to zoom in on one particular theory - the tension myositis syndrome theory of John E. Sarno - so you can have the knowledge and conceptual power to recognise it.
The reason for this is that we keep seeing it and its offspring promoted to people with Long Covid over the last few years. Yet, the community is often unaware of its psychosomatic framework. It isn’t as well-known as The Lightning Process of other brain re-training outfits, but it is as problematic in its psychologisation of illness.
Let’s dig a little deeper…
Understanding TMS: The Foundations of Mind-Body Medicine
Let’s be clear: we don’t support these theories; they are dangerous and insidious. But knowledge is power, and the lack of understanding fuels their promotion by those who are even against psychologisation.
Welcome to Professor Sir Maximus Aurelius Grand High Knight of the Supreme High Simon Wessely’s favourite place - the grey area of medicine.
Dr John E. Sarno was a rehabilitation physician at NYU, and he is the foundation for the ideas and formation of SIRPA. He is a key influence on the beliefs Paul Garner presents, and we need to know our history, as Sarno is one of the earliest and most influential figures behind modern psychosomatic theory.
In the 1980s and 1990s, he developed the ‘diagnosis’ of Tension Myositis Syndrome, now often called Mind-body Syndrome. It is the basis for mind-body medicine and, as Sheldon Cooper would say, it’s hooey. For those at the back, what is the Greek for mind, body?! Yes, psycho, somatic.
He proposed that repressed emotions, especially fear and rage, cause physical symptoms like back pain, migraines, and other chronic issues. Sarno argued that the nervous system and brain generate symptoms as a distraction from unbearable emotions, often unconsciously. A great get-out clause to blame the patient, even if they say this isn’t the case.
But if we are going back to first causes, the Granddaddy of repressive theory and how this links back into psychiatry is Freud. (But that’s another wormhole and wasn't exactly original either - this is a narrative, women especially, have been fighting for aeons!)
Development: Neuroplasticity, Safety, and Pain Science.
Others later expanded Sarno’s ideas using neuroscience and pain psychology. Dr Howard Schubiner (a student of Sarno’s), who we also saw at the SIRPA conference, and Alan Gordon further developed TMS into what is now often referred to as Psychophysiologic Disorders (PDD or Neuroplastic Pain).
These models emphasise that chronic symptoms are real (sound familiar?), brain-generated experiences that are sustained by learned danger signals in the nervous system. This is a key factor in how they are equitable to The Lightning Process and other brain training outfits.
The “fear-safety” dynamic also comes from pain neuroscience, particularly the work of Lorimer Moseley and David Butler, who introduce concepts like pain as a protective mechanism that can become maladaptive.
The idea of recovery requiring a felt sense of safety is also supported by the polyvagal theory of Stephen Porges, which emphasises the autonomic nervous system’s role in detecting safety or threat.
It is this theory of safety and danger that we keep seeing in some Long Covid therapeutic scenarios, in courses and in clinics.
The Myth of Being ‘Stuck in Fight or Flight’
Does fear and safety remind you of anything? Perhaps fight and flight? This is an Aha (and not in the nice Morten Harket way) moment.
We often get told we have symptoms because we are “stuck in fight and flight”, and it is the core tenet of the brain retaining, Lightning Process, Gupta Program bros.
Confusing this with dysautonomia and offering behavioural solutions is not the way to go. There is no scientific evidence that we are ‘stuck in fight or flight’, and we need to understand the origins of this theory.
The triad of Sarno’s TMS theory, pain neuroscience and polyvagal created a conceptual shift that moved the narrative from ‘it’s all in your head’ or ‘you’re imagining it’ to more subtle statements like, ‘you’re in fight and flight, your nervous system just needs to feel safe.’
It sounds more compassionate, but it still relies on the premise that symptoms are perpetuated by perception. In the case of ME and Long Covid, it is particularly dangerous because:
It conflates pathology with psychology - POTS is not a fear response
Invites dubious interventions like brain re-training, somatic therapy, etc
Claims dysautonomia is psychologically driven
Reinforces internalised blame
Invalidates biomedical reality
Replaces objective diagnostic criteria with subjective therapeutic narratives
How Sarno’s Legacy Shows Up Today
Whilst brain re-training programs are more universally recognised as being problematic in Long Covid and ME, these other psychological approaches often fly under the radar. It is important that we recognise them for what they are: medical gaslighting.
The fear-safety model widely promoted in mind-body therapies today has its conceptual roots in Sarno’s theory, but was later shaped by neuroscience and polyvagal theory and can be seen in:
Mind-body syndrome (MBS)
Neuroplastic pain
Psychophysiologic Disorders (PPD)
Central Sensitisation (broader medical overlaps, but not identical)
Pain Reprocessing Therapy (PRT) - developed by Alan Gordon, rooted in similar principles
Mind-Body Syndrome/ Mind-Body Medicine
Functional Somatic Symptoms - in broader psychosomatic medicine
The Dangerous Gap Between Theory and Reality
The problem is that the belief that chronic symptoms are caused and perpetuated by a feeling of danger and or emotional suppression is a conceptual model. High-quality evidence supporting it as a general explanation is totally missing.
TBH, we have serious concerns that these theories are still doing the rounds in Long Covid, usually with a large side-helping of psychosomatic denial. But let’s get into specifics. Why are they harmful?
Firstly, they promote psychologising or blaming the patient, as they imply that symptoms are fully or partially sourced in the patient’s emotional state, thoughts or beliefs.
This can lead to internalised ableism and feelings of guilt and shame. It places a deeply unfair burden on the patient to invest effort into resolving these abnormal beliefs to recover. It also risks pathologising normal emotional responses to chronic illness as the cause rather than the consequences.
In fact, this mind-body theory of chronic pain is already being debunked. Just last week (5th June 2025), the BBC reported on the work of Dr Guy Bewick and Prof Chen, who discovered that chronic pain is physiologically different and is based on a glutamate model. There is also the work of Dr Andreas Goebel in Liverpool, who has found that Fibromyalgia is likely an autoimmune condition.
Respectable Gaslighting: When Compassion Masks Harm
Yet, there is subtlety here as it is often presented as respectable gaslighting, as the danger-safety model sounds compassionate. This is likely the reason for its perpetuation in the Long Covid world and why it goes undetected.
Prematurely assuming psychogenic causes means that biological or physiological factors stop being investigated. It works another way, too, in that in areas where there aren’t many tests or treatments, even if they are believed in, mind-body therapies are resorted to when options run out, especially in the private sphere. This is a false binary and just adds to a monetised industrial complex.
Another false binary is the delineation of safety and illness; this way oversimplifies healing. It ignores biological realities and leads people to wrongly believe that recovery is within their control. This can be alluring, especially if one has recovered, as hooray, you have superpowers and control over nature (not).

Trauma Therapy or Trauma Trade?
The proliferation of these trauma-based, somatic and wider pseudoscience theories means that the model of healing framed as personal responsibility is not challenged. The systemic issues are not dealt with, and it becomes co-opted into a neoliberal narrative of individualisation. A peak example of this is The Lightning Process, with its MLM (multilevel marketing) model.
There seems to be a pattern of people with experience in the wellness industry having Long Covid and then commodifying and specialising in this field and promoting therapies based on Sarno’s TMS theory. (As we were copy editing this it’s come to our attention that Bateman Horne are platforming Brain Training - see Erimatage - we will be writing to them.)
The justification of ‘trying to help people’ is not enough. Personally commodifying nervous system regulation therapies, often at the expense of disabled people’s material needs, isn’t on. However unlikely, we would ask them to have a gentle look in the mirror.
Towards a More Just Model of Care
The central issue is that the mental health of chronically ill people matters, and that we often have to engage with these theories to access mental health support. It would be foolish not to acknowledge that fear, trauma can co-exist with illness, but that doesn’t mean that there are causative links.
We call for informed models of mental health care that centre belief, access and complexity, not emotional correction. There needs to be trauma-informed, patient-led care that does not resort to neuro-gaslighting. Luckily, there are community leaders trying to mobilise a more just model of care, as we can see with Chronic Living Therapy and Remedies. (If you know any more, let us know in the comments.)
We need clinicians supporting chronic illness patients to offer robust mental health support that offers a genuine place where people can receive counselling without having to resort to LLM (although with little on offer, there is an interesting discussion to have about AI providing mental health support to people with energy-limited conditions).
Aspects we would welcome:
Therapists trained in chronic illness literacy and medical trauma.
Language of dysregulation & safety/danger removed.
Focus on navigating distress, trauma, grief and systemic harm, not on symptom elimination.
Validation of emotional pain without assigning it to illness.
Collaborative, not hierarchical clinical practice, where patients set the agenda, with consent-based entry.
Ending of psych referrals for ‘medically unexplained symptoms’
Shift from ‘individual resilience’ to collective responsibility.
Accessible accommodations for people with energy-limited illness.
Recognition that mental health is rooted in social needs being met and assistance with housing, food and financial needs.
Please note: This isn’t an exhaustive list, and if there is anything you feel would be a valued addition, please let us know.
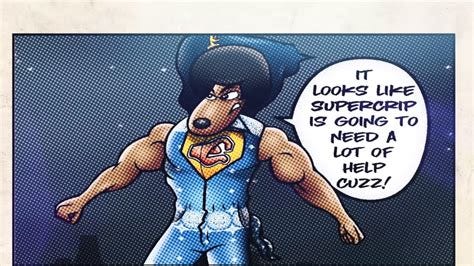
Not Supercrips: A Call for Collective Responsibility
“We are not magically traumatised supercrips who can survive anything, and pretending we are makes us die faster.” Leah Lakshmi Piepzna-Samarasinha, Care Work: Dreaming Disability Justice, 2018.
The irony is that many people with chronic illness have to performatively inform others of their ‘good mental health’ to avoid being blamed for their symptoms. A poignant example of this was Vlad Vexler (sending our best wishes, Vlad), who is experiencing a significant relapse due to a Covid infection. But in the wise words of Piepana-Samarasinha, we are not supercrips who should be able to be ultra-resilient. We should not have to defend our mental health as non-causative.
What is often forgotten is that real safety is collective. It means stable housing, accessible care, respectful providers, freedom from mental coercion and safe mental health care. This includes a benefit system that is fit for purpose for people with Long Covid and ME and based on compassionate principles. So MPs do the right thing and vote against the disability cuts - now and forever. If you didn’t catch LCA in The Guardian commenting on the disastrous benefits bill, here’s the link:
‘Worse than anything under the Tories’: changes to welfare bill anger disability campaigners.’ Frances Ryan.
Watch this space and subscribe to know when our next article drops. As Decode ME approaches we will be prepping a media guide on how to deal with the tricky rhetorical traps we often get faced with. (Phew, philosophy does actually have a use!)






I cannot describe how much I love this article. You’ve comprehensively and solidly debunked this horrible nonsense that has infected the whole of health care and which continues to cause so much damage.
The take issue with only one single point and that is the value of psychological support. If (I recognise it’s a big “if”) psychologists could be relieved of their flawed beliefs and properly trained to support clients with chronic conditions (with or without identified pathology) a lot of good could be done for this isolated and vulnerable group.
👏👏